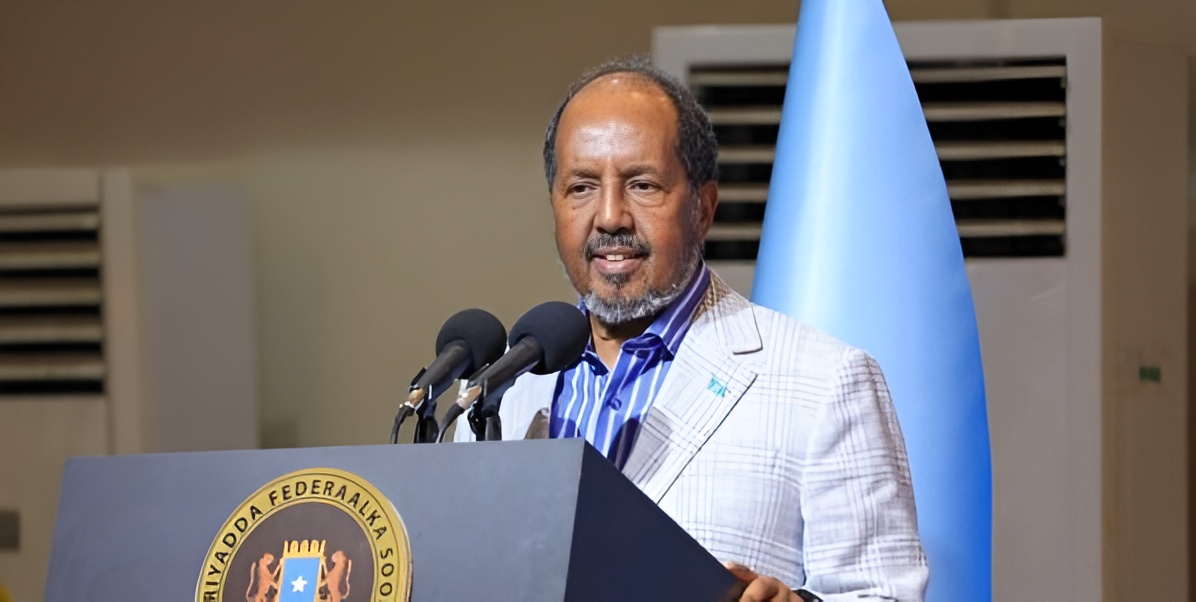
Health CS Duale: SHA to provide Sh550,000 in annual coverage for cancer patients

Duale said reimbursement for intensive care unit and high dependency unit services has been significantly increased, rising from Sh4,480 to Sh28,000 per day.
The government has announced that cancer patients in Kenya will now be eligible for up to Sh550,000 in annual treatment coverage under the Social Health Authority (SHA) programme.
Effective April 1, 2025, these enhanced services will be available to all patients registered with SHA.
More To Read
- Health Ministry clarifies Kenya–US health partnership respects sovereignty, data protection
- KNCHR says Kenyans still locked out of healthcare despite Sh138 billion SHA boost
- Kenya urges stronger regional cooperation as transport corridors fuel disease risks across East Africa
- MPs ditch SHA, the public health scheme they once praised, and opt for private cover
- WHO calls for urgent action to achieve universal health coverage by 2030
- How Trump–Ruto health deal fills the void left after USAID exit
Health Cabinet Secretary Aden Duale confirmed that the coverage would be available to all patients registered with SHA, with funding split between the Social Health Insurance Fund (SHIF) and the Emergency, Chronic, and Critical Illness Fund (ECCIF).
According to Duale, patients will be able to access Sh400,000 through SHIF and an additional Sh150,000 through ECCIF.
"We are thrilled to announce that additional funding has been allocated to enhance the benefits available for patients in need of cancer diagnosis and treatment services. Each patient will now have access up to Sh550,000 per year, specifically designed to support their treatment journey," Duale said.
"Within this framework, Sh400,000 will be available through the SHIF programme and an additional Sh150,000 will be accessible via ECCIF."
ICU and HDU services
Duale said reimbursement for intensive care unit (ICU) and high dependency unit (HDU) services has been significantly increased, rising from Sh4,480 to Sh28,000 per day.
He emphasised that this increase reflects the government's commitment to making critical healthcare services more accessible and adequately supported. Patients will receive these vital services from contracted providers, ensuring they receive the highest quality of care.
"This change underscores our commitment to ensuring that essential healthcare services are accessible and adequately supported,” said the Health CS.
However, the announcement comes amid mounting concerns over the current state of the country's social health insurance system.
There has been widespread public outcry over SHA's implementation of the new health insurance programme.
Since its rollout on October 1, 2024, the system has faced criticism over several issues, including out-of-pocket payments, poor functionality and limited coverage.
Many Kenyans have expressed frustration over their inability to fully benefit from the programme, citing inconsistent experiences with accessing care.
The government's effort to increase healthcare coverage, particularly for cancer and critical care services, is part of its broader commitment to achieving Universal Health Coverage.
However, according to Kenyans, for these improvements to lead to better healthcare for everyone, the government must address the persistent issues within the system. This includes clarifying the roles of SHA, NHIF, and Taifa Care and enhancing the overall effectiveness of the social health insurance programme.
Top Stories Today